Medical research safety is a paramount concern in today’s scientific landscape, particularly in light of recent funding cuts that threaten crucial oversight mechanisms. With the halt of over $2 billion in federal research grants, the ability to protect patient rights and ensure ethical standards during clinical trials is at risk. Institutional Review Boards (IRBs) play an essential role in this protective framework, scrutinizing research proposals to secure the welfare of participants. In an era where research ethics are more critical than ever, the implications of reduced NIH funding cannot be overstated, as they jeopardize not only patient protection in research but also the integrity of the entire scientific process. As stakeholders navigate funding challenges, it is vital to reaffirm our commitment to upholding research participant rights and maintaining the highest ethical standards in clinical research.
The safety and well-being of individuals involved in clinical research is an ongoing challenge that transcends funding issues. As initiatives aimed at ethical medical investigations come under pressure, the significance of oversight systems becomes increasingly apparent. These systems, often overseen by IRBs, are fundamental in guarding the rights of individuals who volunteer for studies, ensuring they are informed and protected throughout the research process. In addition to ethical considerations, there is an urgent need to address the consequences stemming from reduced governmental support for critical health research. By fostering a culture that prioritizes participant safety, we can advocate for robust policies that enhance the integrity of research while mitigating risks associated with funding deficiencies.
The Impact of NIH Funding Cuts on Medical Research Safety
The recent funding cuts from the National Institutes of Health (NIH) have raised significant concerns regarding medical research safety. These cuts threaten the fundamental framework that governs human subject research through institutional review boards (IRBs), which are critical in ensuring ethical compliance and patient protection. Without adequate funding, the capacity of IRBs to effectively monitor and oversee clinical trials diminishes, potentially leading to the increased risk of ethical breaches and unresolved participant rights issues. The halt in resources directly jeopardizes not only the ongoing trials but also the public trust that is essential for successful research endeavors.
Moreover, the suspension of over $2 billion in funding has ripple effects that extend beyond immediate oversight concerns. It hampers the ability to train and support the investigators who design and conduct these trials. As a result, research institutions may struggle to maintain the rigorous standards necessary for safeguarding patient well-being. These breaches in safety protocols can lead to adverse events and unethical conduct that might go unchecked, thereby undermining decades of progress in clinical trial ethics and patient protection measures.
Understanding the Role of Institutional Review Boards (IRBs)
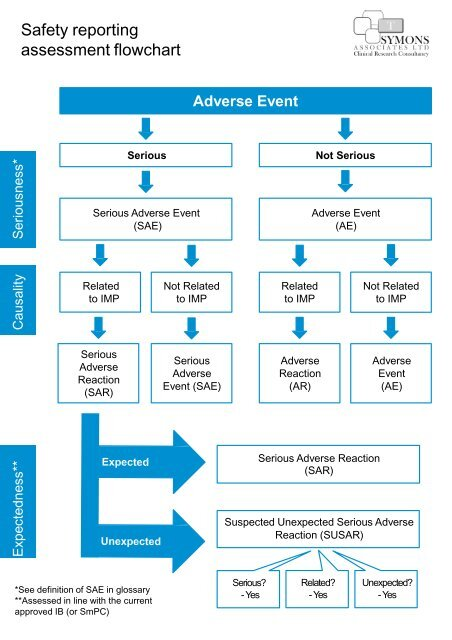
Institutional Review Boards (IRBs) play a pivotal role in the landscape of medical research, serving as the ethical backbone that ensures compliance with research regulations and protects participant rights. Their responsibilities include thorough evaluations of research proposals, assessing the safety and welfare of participants, and ensuring that informed consent processes are properly implemented. This structure not only safeguards participants from harm but also fortifies the integrity of the research processes in academic and clinical settings. The recent reduction in NIH funding raises alarm about the operational capacity of IRBs, which may be forced to cut back on essential services and resources.
In the context of collaborative research, IRBs facilitate unity and compliance across multiple institutions. They look at potential risks and benefits, and apply lessons learned from past ethical violations in medical research history. With sufficient funding, IRBs can sustain their critical advisory and monitoring roles, ensuring that research projects adhere to established ethical guidelines. Thus, as funding diminishes, the repercussions are felt not just by research organizations but also by the communities that rely on ethical medical research for advancements in health care.
Patient Protection in Research: An Urgent Necessity
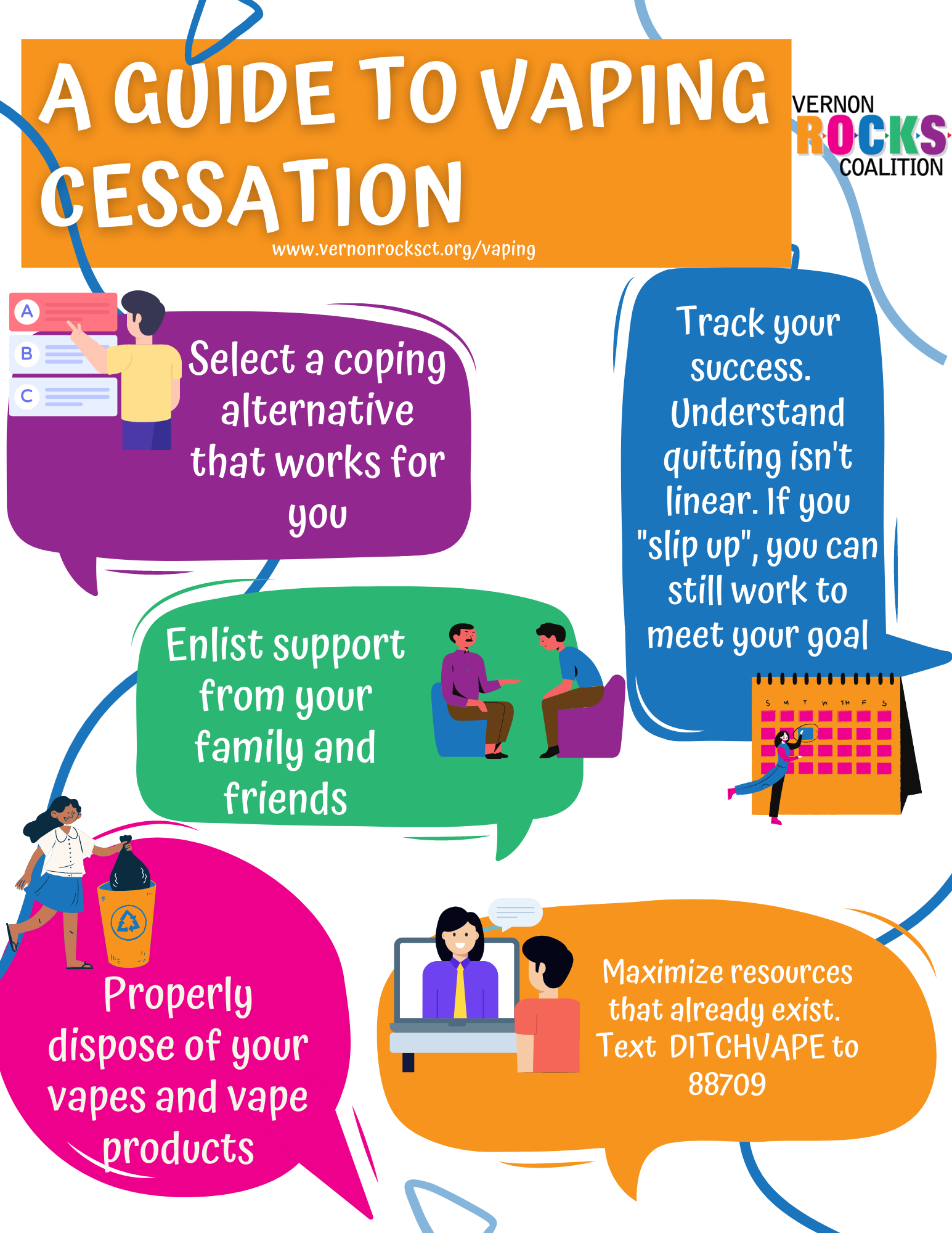
The safety of patients participating in research is non-negotiable, making robust patient protection mechanisms an urgent necessity. Participants must be adequately informed about the risks and benefits associated with studies; this empowerment is largely orchestrated by the oversight of IRBs. However, funding cuts have the potential to compromise these safeguards, as the resources available for proper training, community outreach, and participant communication may dwindle. As history has shown, failure to prioritize the protection of research participants can lead to disastrous outcomes, which is why sustaining these protective measures through adequate funding is paramount.
Enhanced patient protection not only preserves participant rights but also fosters community trust in clinical research. Engaging diverse populations in research studies necessitates transparent communication regarding participant rights and safety protocols. When patients perceive that their safety is compromised, public skepticism can grow, leading to decreased participation in essential research. The ongoing NIH funding cuts exacerbate these concerns, putting at risk not only the safety of current participants but also the future of clinical trials designed to advance health solutions.
Challenges Facing Multisite Research Collaborations
As the landscape of medical research evolves to encompass multisite collaborations, the availability of federal funding becomes increasingly critical for success. These collaborations allow for the pooling of resources, expertise, and patient populations to tackle complex health issues, such as Alzheimer’s disease. The SMART IRB initiative previously alleviated many challenges inherent in multisite research by streamlining the review process. However, with the recent halt of funding, these collaborative efforts face significant obstacles, as new sites and studies are unable to proceed, hampering innovative progress in critical research areas.
Additionally, the impact of halted collaborations extends to the quality of the studies being conducted. The reduction in funding limits the scope of engagement with diverse patient populations, which is vital for ensuring that findings are applicable and beneficial across different demographics. This narrowing of the research pool not only affects statistical validity but could also lead to biased outcomes that fail to adequately represent varied health needs. All these challenges culminate in a precarious situation, threatening the advancements in medical science that depend heavily on successful multisite collaborations.
Historical Context: Learning from Past Medical Misdemeanors
Understanding the historical context of medical research oversight is essential to appreciate the role of IRBs in patient protection. Historical misdeeds, such as the Tuskegee Syphilis Study and the unethical use of vulnerable populations in clinical trials, underscore the necessity of robust ethical frameworks in research. These events have shaped current regulations and epitomized the importance of informed consent and respect for participant rights. However, the ongoing funding cuts threaten to erode the standards established in response to these historical transgressions.
Today, as IRBs face financial constraints, the risk of repeating history looms larger. Unmonitored studies could potentially repeat past errors if oversight becomes lax due to resource shortages. Ensuring ethical research requires continuous improvement of policies and practices grounded in lessons learned from history. Thus, advocacy for sustained funding is critical not only for present integrity in research but also for honoring the commitment to never repeat the mistakes of the past.
The Necessity of Ethical Oversight in Clinical Trials
Ethical oversight is the cornerstone of clinical trials, ensuring that medical research adheres to established guidelines designed to protect participants. Research environments are required to maintain comprehensive ethical standards and accountability, which can only be achieved through diligent oversight. Given recent financial setbacks, the functioning of IRBs as the ethical watchdogs of clinical trials has come into question. Without sufficient support and funding, the ability to uphold these high ethical standards may falter.
Moreover, robust ethical oversight instills confidence in research participants, encouraging them to volunteer for studies knowing that their rights and well-being are safeguarded. This confidence is particularly crucial in sensitive domains such as clinical trials for new medications or treatments. The future health of research institutions, and by extension, public health at large, hinges on the institutions’ ability to maintain ethical oversight amidst ongoing financial pressures. Ensuring adequate funding for these oversight mechanisms is necessary to protect the integrity and advancement of medical research.
Navigating the Ethical Landscape of Clinical Trials
Navigating the ethical landscape of clinical trials requires a thorough understanding of both the historical context and current challenges faced by research institutions. The ethical considerations surrounding participant rights, informed consent, and minimization of harm are at the forefront of research design and implementation. With research participants often coming from vulnerable populations, maintaining ethical standards is critical to uphold public trust and ensure that the rights of all individuals involved are respected and protected.
In light of recent funding constraints, the capacity of research institutions to navigate these complex ethical dilemmas has become increasingly precarious. Any disruptions in funding can adversely impact the ability to train staff, implement best practices, and maintain thorough review processes conducted by IRBs. Therefore, proactive measures are essential to advocate for continued support of ethical oversight mechanisms that are fundamental to maintaining high standards of conduct in clinical research.
The Future of Research Funding and Ethical Oversight
Looking ahead, the future of research funding and ethical oversight is fraught with uncertainty due to potential cuts in federal support. As institutions strive to innovate and advance medical knowledge, the reliance on consistent funding streams remains paramount. The interruption of grants and contracts can halt vital research activities, challenging the ability of IRBs to function effectively and uphold their ethical obligations to protect participants. Thus, advocacy for funding restoration is crucial to ensure both the advancement of research and the protection of patient rights.
Moreover, as other funding avenues and partnerships are explored, there is a pressing need for transparency and ethics in all funding applications and collaborations. Balancing fiscal realities with the ethical imperatives of patient protection requires vigilance and commitment from all stakeholders in the research enterprise. The integrity of future medical advancements hinges on maintaining robust ethical oversight throughout every stage of research, emphasizing the necessity of sustained support for these critical frameworks.
Frequently Asked Questions
What is the role of IRB oversight in ensuring medical research safety?
Institutional Review Board (IRB) oversight is critical in maintaining medical research safety. IRBs meticulously review research proposals to ensure the rights and welfare of human participants are safeguarded, evaluating factors such as study design, informed consent processes, risk assessments, and participant safety protocols. This rigorous oversight helps prevent potential harm from unethical research practices.
How do NIH funding cuts impact patient protection in research?
NIH funding cuts significantly jeopardize patient protection in research by hindering the operational capacity of IRBs, which are essential for overseeing ethical research practices. Decreased funding may lead to fewer resources for monitoring studies, resulting in potential safety risks for research participants and undermining public trust in clinical trials.
What are the key research participant rights protected by clinical trial ethics?
Clinical trial ethics are designed to uphold crucial research participant rights, including the right to informed consent, privacy, and the right to withdraw from the study at any time without penalty. These ethics ensure that participants are fully aware of the study’s risks and benefits, promoting their safety and autonomy throughout the research process.
Why is IRB oversight vital for ethical medical research?
IRB oversight is vital for ethical medical research as it serves as a system of checks and balances. By reviewing studies from multiple angles—such as risk management, informed consent, and participant safety—IRBs ensure that research aligns with ethical standards, protecting participants from harm and promoting ethical integrity within the research community.
How do historical events shape today’s patient protection policies in medical research?
Historical events, such as the Tuskegee syphilis study and unethical experiments during World War II, have profoundly influenced today’s patient protection policies in medical research. These tragedies highlighted the need for stringent oversight, leading to the establishment of IRBs and federal regulations aimed at ensuring participant safety, informed consent, and ethical conduct in research.
What challenges can halt research and endanger patient safety in clinical trials?
Challenges such as funding cuts, bureaucratic delays, and administrative barriers can halt research initiatives, endangering patient safety in clinical trials. When studies are paused or canceled, existing participants may not receive necessary care, and potential benefits of the research may be lost, ultimately affecting public trust in medical research.
How does SMART IRB facilitate patient safety across multiple research sites?
SMART IRB streamlines patient safety across multiple research sites by allowing a single IRB to oversee a multi-site clinical trial, thus reducing duplication of efforts and ensuring consistent ethical standards. This system enhances collaboration among institutions, facilitates timely participant recruitment, and strengthens protections for those involved in research studies.
| Key Point | Details |
|---|---|
| Funding Cuts | The Trump administration’s freeze of over $2 billion in federal research grants has disrupted patient safety efforts. |
| Impact of SMART IRB | SMART IRB is crucial for ensuring effective oversight in multi-site studies but is currently hindered by funding restrictions. |
| Role of IRBs | Institutional Review Boards (IRBs) review research proposals to protect patient rights and welfare during studies. |
| Historical Lessons | Past medical abuses have shaped the IRB system to protect participants in medical research. |
| Consequences of Halts | Halting studies can undermine public trust in medical research and harm ongoing collaborations. |
Summary
Medical research safety is crucial to ensuring the well-being of participants involved in clinical studies. The recent funding cuts imposed on federal research grants not only undermine the integrity of medical research but also jeopardize the safety and rights of patients. Such disruptions to essential oversight mechanisms like the SMART IRB have serious implications for public trust and the effectiveness of collaborative research. Continued support and sound funding for medical research are vital for safeguarding participants and advancing scientific inquiry.