Maternal mortality remains a pressing issue in the United States, where the incidence of pregnancy-related deaths has been alarmingly on the rise. In fact, recent studies indicate that the U.S. leads other high-income nations in maternal mortality rates, highlighting significant gaps in U.S. maternal health care. The devastating reality is that over 80 percent of these deaths are preventable, underscoring the urgent need for improved prenatal and postpartum care systems. Racial disparities in maternal health are particularly pronounced, with American Indian, Alaska Native, and Black women facing disproportionately higher risks. Moreover, factors such as cardiovascular disease complicate pregnancy, posing further threats to maternal well-being and emphasizing the critical need for focused interventions.
The term “maternal mortality” encompasses the tragic outcomes of pregnancy-related deaths, but it can also be understood as broader implications related to maternal health crises. This includes understanding pregnancy-related fatalities as part of the ongoing discourse on healthcare Quality for expectant mothers. The rise in such fatalities raises questions not only about systemic healthcare failures but also about the socioeconomic factors influencing maternal outcomes. Issues such as inadequate postpartum care, disparities based on race, and the increasing relevance of cardiovascular health during pregnancy are vital to this discussion. Recognizing these interconnected aspects can help pave the way for comprehensive policy changes and improved healthcare strategies to safeguard maternal health effectively.
The Alarming Rise in U.S. Maternal Mortality Rates
The United States has recently faced a concerning upward trend in maternal mortality rates, a statistic that underscores a serious public health crisis. A significant finding reveals that between 2018 and 2022, the maternal mortality rate increased from 25.3 to 32.6 deaths per 100,000 live births. This stark contrast highlights the urgent need for public health interventions and a reassessment of the healthcare infrastructure surrounding maternal care. The ongoing rise, particularly during the COVID-19 pandemic, has exacerbated the vulnerability of pregnant individuals, especially those from marginalized communities.
Moreover, the statistics point to preventable deaths, given that over 80% of pregnancy-related deaths could have been avoided with improved health systems and care practices. The disparities in rates among different racial groups add another layer of complexity, as American Indian, Alaska Native, and non-Hispanic Black women face significantly higher mortality rates than their white counterparts. These inequities provoke a call to action to address systemic healthcare inadequacies and create comprehensive strategies to enhance maternal health outcomes across the nation.
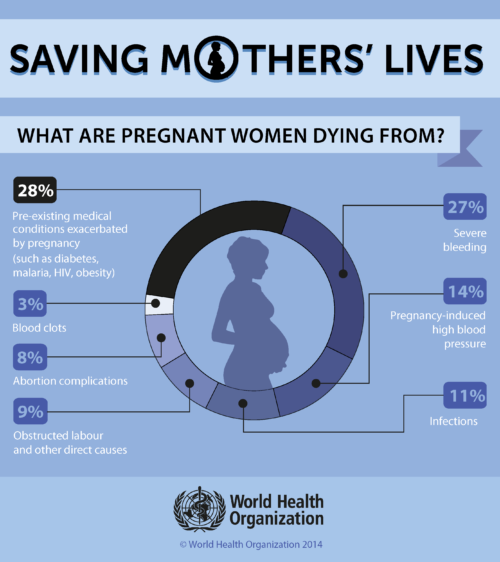
Understanding Pregnancy-Related Deaths and their Causes
Pregnancy-related deaths in the U.S. can be attributed to a convergence of factors, including healthcare access, quality of maternal care, and the prevalence of chronic health conditions such as cardiovascular disease. Over 20% of pregnancy-related deaths are due to cardiovascular issues, which are increasingly affecting women at younger ages. This troubling trend indicates a greater need for awareness and proactive management of cardiovascular health in reproductive-age women. As medical professionals point out, the transition of cardiovascular disease to the leading cause of maternal mortality signals a significant shift in maternal health dynamics.
In addition to cardiovascular concerns, disparities in healthcare access contribute to varying rates of pregnancy-related deaths across racial lines. While some states demonstrate successful models in reducing maternal mortality, others lag significantly behind. The implications stress the need for equitable policies and improved healthcare systems that not only address prenatal care but also extend into the postpartum phase, where many deaths currently occur. By understanding the underlying reasons for these deaths, healthcare providers can better navigate solutions that focus on comprehensive maternal health.
The Role of Postpartum Care in Maternal Health
Postpartum care plays a critical role in influencing maternal health outcomes, yet it often remains inadequately addressed in U.S. healthcare systems. Most traditional models focus on the initial weeks after delivery, overlooking the importance of continuous support in the months that follow. Recent studies illustrate that nearly one-third of maternal deaths occur between 42 days and one year postpartum, highlighting the necessity of prolonged healthcare services. The transition period marks a vulnerable phase where new mothers require comprehensive support for both physical and mental health.
To mitigate risks associated with late maternal deaths, it is essential to redefine postpartum care as a continuum rather than a finite period ending at six weeks postpartum. Optimizing this could result in significant improvements in maternal health outcomes. Initiatives aimed at extending postpartum services can help address conditions such as cardiovascular disease that may develop or worsen during this period. By fostering a holistic approach to postpartum care, healthcare systems can proactively manage the well-being of mothers, ultimately reducing pregnancy-related deaths and enhancing the overall health of women.
Racial Disparities in Maternal Health Outcomes
Racial disparities in maternal health outcomes persist as a daunting challenge within the U.S. healthcare landscape. The alarming statistic that American Indian and Alaska Native women experience pregnancy-related deaths at nearly four times the rate of white women demands immediate attention. Such inequities reflect broader systemic issues in access to quality healthcare, highlighting the need for targeted interventions that address the unique challenges faced by these populations. Studies consistently indicate that factors such as systemic bias, discrimination, and inadequate access to prenatal and postpartum care contribute to these disparities.
Efforts to bridge the gap in maternal health outcomes must focus on eliminating barriers that hinder access to timely and effective care. Strategies may involve increasing funding for community health initiatives, employing culturally competent healthcare providers, and advocating for policies that support at-risk populations. By taking a comprehensive approach that acknowledges the complexity of racial disparities in maternal health, stakeholders can work collaboratively to implement effective solutions that improve outcomes for all mothers across the racial spectrum.
Innovations Needed to Reduce Maternal Mortality
Innovative solutions are essential in combatting the concerning rates of maternal mortality seen in the U.S. healthcare system today. Research indicates that significant improvements could potentially be achieved in maternal health outcomes through the refinement of care models in both prenatal and extended postpartum settings. New strategies must focus on proactive measures that enhance overall healthcare quality and access, particularly in underserved communities where the risks are disproportionately high. Adopting evidence-based practices, integrating telehealth services, and employing advanced data tracking technologies are just a few examples of innovative measures that could lead to better maternal health outcomes.
Additionally, embracing community-based programs that foster collaboration among healthcare providers, families, and local organizations can create a more robust support network for expectant and new mothers. By prioritizing maternal health as a crucial component of public health, particularly during periods of vulnerability, and harnessing innovation to improve care delivery, healthcare systems can effectively work towards reducing preventable pregnancy-related deaths in the U.S. Sustained investment in these innovations is invaluable for ensuring that all mothers receive the quality care they deserve.
The Impact of Cardiovascular Disease on Pregnancy Outcomes
Cardiovascular disease has emerged as a leading cause of pregnancy-related mortality, significantly impacting maternal health during and after pregnancy. The increasing prevalence of hypertension, pre-eclampsia, and other cardiovascular conditions among younger women raises alarm bells for healthcare practitioners. Understanding the risk factors for cardiovascular complications during pregnancy is vital for developing effective intervention strategies that can save lives. As rates of chronic health conditions continue to rise, it becomes increasingly crucial to emphasize the importance of cardiovascular health during preconception care and throughout the perinatal period.
The relationship between cardiovascular disease and pregnancy outcomes necessitates comprehensive healthcare and monitoring for women throughout their reproductive years. Healthcare providers must engage in education and outreach, enabling young women to adopt healthier lifestyles and manage risk factors before and during pregnancy. By prioritizing cardiovascular health and integrating continuous screening into women’s healthcare, the healthcare system can create pathways that effectively reduce maternal mortality rates attributed to cardiovascular complications.
Enhancing Access to Maternity Care Services
Access to comprehensive maternity care services is essential for improving maternal health outcomes and preventing pregnancy-related deaths. Many expectant mothers, particularly those in rural or underserved communities, face significant hurdles in obtaining prenatal and postpartum care. Addressing these barriers requires urgent action from policymakers who must advocate for and invest in healthcare infrastructures that ensure equitable access to quality services. Initiatives that promote telehealth and mobile clinics are promising approaches that can help reach mothers who otherwise remain isolated from essential maternal healthcare.
By enhancing access to maternity care services, especially in areas with high rates of maternal mortality, we can create sustainable pathways for women and their families. The integration of community outreach programs can provide education and resources, empowering mothers to seek care proactively. Health systems should focus on establishing partnerships with community organizations to facilitate support networks, bridging gaps in care, and ensuring continuous engagement from pregnancy through the postpartum period. Investing in accessible maternity care will play a formative role in reversing current trends in maternal mortality.
The Importance of Quality Care in Pregnancy
Quality care during pregnancy is crucial not only for the health of the mother but also for the development of the fetus. The need for high standards of care throughout prenatal visits cannot be overstated, as these early encounters offer opportunities to assess risks, educate mothers, and intervene when necessary. Quality care involves comprehensive assessment practices that ensure any chronic conditions, such as cardiovascular issues, are managed effectively before and during pregnancy. Enhancements in training for healthcare providers focused on both clinical and interpersonal skills can foster better communication and trust, leading to improved maternal health outcomes.
In addition to excellent prenatal care, ongoing support needs to be a priority in the postpartum phase, where many maternal deaths occur. Developing protocols that ensure mothers receive follow-up care tailored to their specific needs can aid in early recognition and management of complications. Furthermore, fostering a supportive healthcare environment that encourages mothers to voice their concerns will drive better engagement with healthcare systems. Prioritizing quality care within all aspects of maternal health will ultimately be instrumental in reducing the prevalence of pregnancy-related deaths.
Future Directions in Maternal Health Research
Future research in maternal health must address ongoing issues in mortality rates and inequalities within healthcare access. As the data from recent studies highlight, identifying the multifaceted causes of maternal mortality is paramount for informing targeted interventions. Initiatives should focus on not only improving prenatal and postpartum care but also deeply exploring the social determinants of health that impact maternal wellbeing. Larger datasets and longitudinal studies can provide insights into the effectiveness of systemic changes aimed at reducing disparities in maternal health outcomes.
Moreover, there’s an urgent need for research funding to explore innovative strategies for enhancing care delivery models across various demographic groups. By championing interdisciplinary research that encompasses obstetrics, public health, and social sciences, scholars and practitioners can work collaboratively towards practical solutions. The call to prioritize maternal health through informed research will play a significant role in shaping policies that focus on improving the lives of mothers and their families.
Frequently Asked Questions
What are the main causes of maternal mortality in the U.S. during pregnancy and postpartum?
In the U.S., the leading causes of maternal mortality include cardiovascular disease, hemorrhage, and infections, with cardiovascular disease accounting for over 20% of pregnancy-related deaths. Chronic conditions such as hypertension have become increasingly common among pregnant individuals, contributing to the rise in maternal mortality rates.
How do racial disparities impact maternal mortality rates in the United States?
Racial disparities significantly affect maternal mortality rates in the U.S., with American Indian and Alaska Native women facing the highest rates. Non-Hispanic Black women also experience disproportionately high pregnancy-related deaths compared to their white counterparts, highlighting the systemic inequities present in U.S. maternal health care.
What defines late maternal deaths and why are they significant in studying maternal mortality?
Late maternal deaths refer to deaths occurring between 42 days and one year after pregnancy. They are significant because they account for nearly a third of all maternal deaths, indicating that postpartum care must address health challenges beyond the traditional six-week follow-up period.
How has the COVID-19 pandemic influenced trends in maternal mortality in the U.S.?
The COVID-19 pandemic has influenced trends in maternal mortality, particularly in 2021 when a sharp increase in deaths was observed. Overall, maternal mortality rates have risen continuously between 2018 and 2022, suggesting that the pandemic exacerbated existing health disparities and challenges in maternal care.
What initiatives could potentially reduce maternal mortality rates in the U.S.?
Potential initiatives to reduce maternal mortality rates include improving access to quality prenatal and postpartum care, increasing public health investments, addressing systemic biases in healthcare, and implementing policies that standardize care across states to mitigate disparities in maternal health.
Why is it important to include cardio-related issues in postpartum maternal health discussions?
Including cardiovascular issues in postpartum maternal health discussions is critical as these conditions are becoming leading causes of pregnancy-related deaths. Acknowledging and addressing these health challenges can lead to more comprehensive care strategies that support the health of mothers beyond birth.
What role does public health infrastructure play in addressing maternal mortality?
Public health infrastructure plays a crucial role in addressing maternal mortality by enabling consistent tracking of maternal deaths, informing policy improvements, and providing resources for quality care. Continued investment in this infrastructure is vital to reversing rising maternal mortality trends.
| Key Points | Details |
|---|---|
| Rising Maternal Mortality Rates | The U.S. continues to have the highest maternal mortality rate among high-income countries, with rates rising from 25.3 to 32.6 deaths per 100,000 live births between 2018 and 2022. |
| Preventable Deaths | Over 80% of pregnancy-related deaths in the U.S. are preventable. |
| Significant Racial Disparities | American Indian and Alaska Native women experience the highest mortality rates, nearly four times that of white women. |
| COVID-19 Impact | The sharpest increase in maternal mortality was observed in 2021, reflecting challenges posed by the COVID-19 pandemic. |
| Role of Chronic Conditions | Chronic medical conditions such as cardiovascular disease are increasingly affecting younger pregnant individuals. |
| Late Maternal Deaths | Late maternal deaths, which occur between 42 days and 1 year post-delivery, need to be recognized as a significant issue. |
Summary
Maternal mortality remains a critical public health issue in the U.S., with the country leading high-income nations in related deaths. The alarming rise in rates, particularly during the COVID-19 pandemic, highlights the urgent need for systemic changes in healthcare. Addressing disparities and investing in better prenatal and postpartum care are essential steps toward preventing these tragic losses. With more than 80% of these deaths deemed preventable, it is imperative that policymakers prioritize maternal health to ensure safer outcomes for all expectant mothers.